By Dr. Vivek V Gumaste, MD, MRCP(I), MHCM (Harvard)
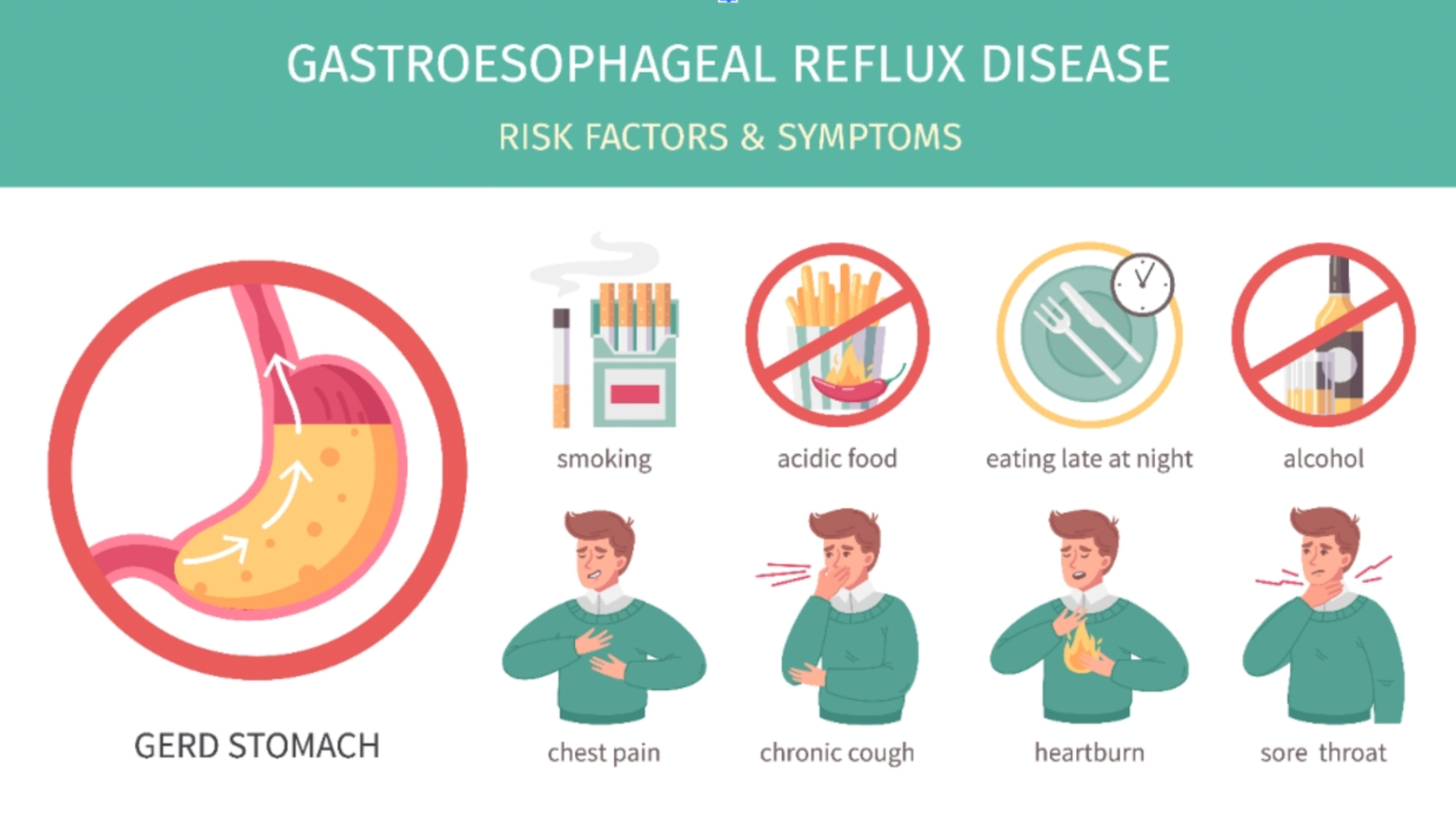
Gastroesophageal Reflux Disease (GERD) is a common digestive condition that affects about 1 in 4 people in North America. It causes symptoms like heartburn, regurgitation, and chest discomfort. But GERD isn’t just inconvenient, it’s costly and potentially dangerous. Over 4.3 million outpatient visits are made annually for GERD in the U.S., with an average treatment cost of $12,232 per patient. Of this, $4,277 is spent on medications alone.
GERD also increases the risk of developing esophageal cancer. Despite this, many patients don’t respond well to standard treatments like proton pump inhibitors (PPIs). Studies show that up to 50% of people taking PPIs still experience symptoms. Clearly, new solutions are needed
Limitations of Current Testing
Diagnosing GERD can be challenging. Endoscopy often shows normal results, even in symptomatic patients. pH testing, while considered a gold standard, has a high false-negative rate and is uncomfortable. Intraluminal impedance testing adds some value but is still invasive and difficult for patients.
A New Approach: Mucosal Impedance Testing (MIT)
A promising development discussed in wellness forum health communities is Mucosal Impedance Testing (MIT). This method measures the health of the esophageal lining in real time, during an endoscopy. It can identify both acid and non-acid reflux and detect long-term tissue damage. The MiVu device, developed by Diversatek Healthcare, uses a sensor placed on the endoscope to gather data. Studies show MIT may be more accurate than traditional pH tests and is easier on patients.
Could Your Genes Be Behind Your Heartburn?
Genetics also play a big role in GERD. Research shows that 30–40% of GERD risk is inherited. Specific genes, such as FOXF1 and BARX1, have been linked to the disease. These genes may affect how the esophagus develops and functions. There’s also strong genetic overlap between GERD, Barrett’s esophagus, and esophageal cancer, highlighting the need for early detection and tailored treatment.
Precision Medicine and PPIs
PPIs are broken down in the liver by an enzyme called CYP2C19. Depending on a person’s genes, the body may process the drug too quickly or too slowly. Genetic testing (genotyping) can help doctors personalize PPI doses. However, this practice is not yet common in routine care. Summit Healthcare Solutions suggests more clear guidelines are needed before it becomes widespread.
What About Probiotics?
Probiotics are often used for gut health, and some small studies suggest they may help with GERD symptoms like bloating and regurgitation. However, more large-scale, high-quality research is needed to confirm these benefits.
AI and New Drugs
Artificial intelligence (AI) is being used to read diagnostic images, interpret test results, and speed up drug discovery. In Japan, researchers developed a new drug candidate (DQ-18) using AI, showing faster and safer results.
A newly approved drug, Voquezna (vonoprazan), offers quicker relief than PPIs. It works differently and does not need food for activation. Studies show it may be more effective for GERD and peptic ulcers.
The Growing GERD Market
According to Summit Healthcare Solutions, the GERD market in major global regions was worth $5.1 billion in 2024 and could grow to $6.4 billion by 2035. New technology, personalized care, and better drugs are driving this growth.
Final Thoughts
GERD is more than just acid reflux. From genetics and new testing methods to AI and advanced drugs, the future of GERD treatment is rapidly evolving. With better tools and tailored care, millions of patients could finally find lasting relief.